1 Tupper KW, Wood E, Yensen R, Johnson MW. Psychedelic medicine: a re-emerging therapeutic paradigm. CMAJ. 2015;187(14):1054–9.
2 Schultes RE, Hofmann A, Rätsch C. Plants of the Gods: Their Sacred, Healing, and Hallucinogenic Powers. 2nd ed. Rochester, Vt: Healing Arts Press; 2001.
3 Passie T, Halpern JH, Stichtenoth DO, Emrich HM, Hintzen A. The pharmacology of lysergic acid diethylamide: a review. CNS Neurosci Ther. 2008;14(4):295–314.
4 Dumont GJH, Sweep FCGJ, van der Steen R, Hermsen R, Donders ART, Touw DJ, et al. Increased oxytocin concentrations and prosocial feelings in humans after ecstasy (3,4-methylenedioxymethamphetamine) administration. Soc Neurosci. 2009;4(4):359–66.
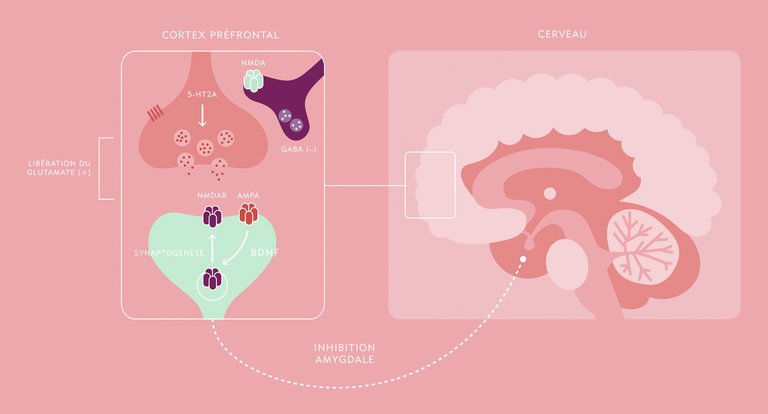
5 Hashimoto K. The role of glutamate on the action of antidepressants. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(7):1558–68.
6 Vollenweider FX, Kometer M. The neurobiology of psychedelic drugs: implications for the treatment of mood disorders. Nat Rev Neurosci. 2010;11(9):642–51.
7 Baumeister D, Barnes G, Giaroli G, Tracy D. Classical hallucinogens as antidepressants? A review of pharmacodynamics and putative clinical roles. Ther Adv Psychopharmacol. 2014;4(4):156–69.
8 Caddy C, Giaroli G, White TP, Shergill SS, Tracy DK. Ketamine as the prototype glutamatergic antidepressant: pharmacodynamic actions, and a systematic review and meta-analysis of efficacy. Ther Adv Psychopharmacol. 2014;4(2):75–99.
9 Duman RS. Pathophysiology of depression and innovative treatments: remodeling glutamatergic synaptic connections. Dialogues Clin Neurosci. 2014;16(1):11–27.
10 Bogenschutz MP, Johnson MW. Classic hallucinogens in the treatment of addictions. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:250–8.
11 Carhart-Harris RL, Muthukumaraswamy SD, Roseman L, Kaelen M, Droog W, Murphy K, et al. Neural correlates of the LSD experience revealed by multimodal neuroimaging. Proc Natl Acad Sci USA. 2016;113(17):4853–8.
12 Muthukumaraswamy SD, Carhart-Harris RL, Moran RJ, Brookes MJ, Williams TM, Errtizoe D, et al. Broadband cortical desynchronization underlies the human psychedelic state. J Neurosci. 2013;33(38):15171–83.
13 Tagliazucchi E, Roseman L, Kaelen M, Orban C, Muthukumaraswamy SD, Murphy K, et al. Increased Global Functional Connectivity Correlates with LSD-Induced Ego Dissolution. Curr Biol. 2016;26(8):1043–50.
14 Palhano-Fontes F, Andrade KC, Tofoli LF, Santos AfC, Crippa JAS, Hallak JEC, et al. The psychedelic state induced by ayahuasca modulates the activity and connectivity of the default mode network. PLoS One. 2015;10(2):e0118143.
15 Carhart-Harris RL, Leech R, Hellyer PJ, Shanahan M, Feilding A, Tagliazucchi E, et al. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci. 2014;8:20.
16 Hasler F, Grimberg U, Benz MA, Huber T, Vollenweider FX. Acute psychological and physiological effects of psilocybin in healthy humans: a double-blind, placebo-controlled dose-effect study. Psychopharmacology (Berl). 2004;172(2):145–56.
17 Grof S. Realms of the human unconscious: Observations from LSD research. New York: Viking Press; 1975.
18 Griffiths RR, Richards WA, McCann UD, Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology (Berl). 2006;187(3):268–83.
19 Griffiths RR, Richards WA, Johnson MW, McCann UD, Jesse R. Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. J Psychopharmacol (Oxford). 2008;22(6):621–32.
20 MacLean KA, Johnson MW, Griffiths RR. Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. J Psychopharmacol. 2011;25(11):1453–61.
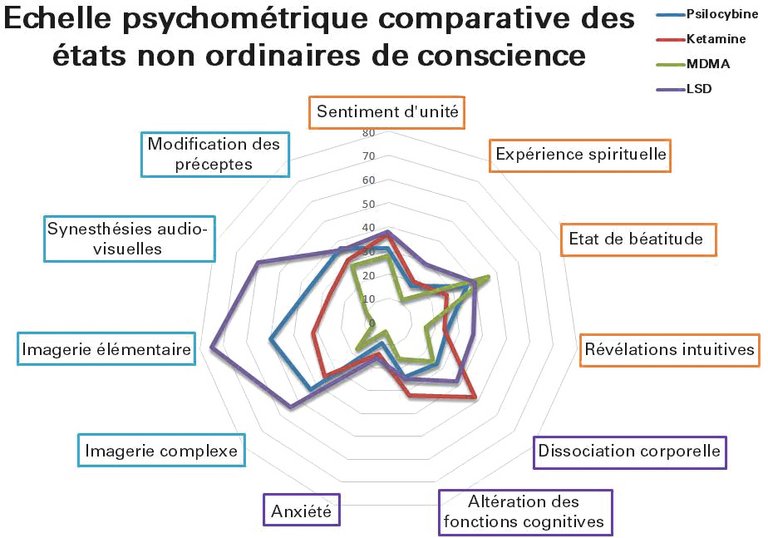
21 Studerus E, Gamma A, Vollenweider FX. Psychometric evaluation of the altered states of consciousness rating scale (OAV). PLoS One. 2010;5(8):e12412. [fnei].
22 Passie T, Seifert J, Schneider U, Emrich HM. The pharmacology of psilocybin. Addict Biol. 2002;7(4):357–64.
23 Carhart-Harris RL, Kaelen M, Bolstridge M, Williams TM, Williams LT, Underwood R, et al. The paradoxical psychological effects of lysergic acid diethylamide (LSD). Psychol Med. 2016;46(7):1379–90.
24 Emerson A, Ponté L, Jerome L, Doblin R. History and future of the Multidisciplinary Association for Psychedelic Studies (MAPS). J Psychoactive Drugs. 2014;46(1):27–36.
25 Cohen S. Lysergic acid diethylamide: side effects and complications. J Nerv Ment Dis. 1960;130:30–40.
26 Strassman RJ. Adverse reactions to psychedelic drugs. A review of the literature. J Nerv Ment Dis. 1984;172(10):577–95.
27 Halpern JH, Pope HG. Do hallucinogens cause residual neuropsychological toxicity? Drug Alcohol Depend. 1999;53(3):247–56.
28 Tylš F, Páleníček T, Horáček J. Psilocybin – Summary of knowledge and new perspectives. Eur Neuropsychopharmacol. 2014;24(3):342–56.
29 Studerus E, Gamma A, Kometer M, Vollenweider FX. Prediction of psilocybin response in healthy volunteers. PLoS One. 2012;7(2):e30800.
30 Johnson M, Richards W, Griffiths R. Human hallucinogen research: guidelines for safety. J Psychopharmacol (Oxford). 2008;22(6):603–20.
31 Grob C. MDMA research: preliminary investigations with human subjects. Int J Drug Policy. 1998;9(2):119–24.
32 Burgess C, O’Donohoe A, Gill M. Agony and ecstasy: a review of MDMA effects and toxicity. Eur Psychiatry. 2000;15(5):287–94.
33 Perry EB, Cramer JA, Cho H-S, Petrakis IL, Karper LP, Genovese A, et al. Psychiatric safety of ketamine in psychopharmacology research. Psychopharmacology (Berl). 2007;192(2):253–60.
34 Wang C, Zheng D, Xu J, Lam W, Yew DT. Brain damages in ketamine addicts as revealed by magnetic resonance imaging. Front Neuroanat. 2013;7:23.
35 Morgan CJA, Curran HV. Ketamine use: a review. Addiction. 2012;107(1):27–38.
36 Dos Santos RG. Safety and side effects of ayahuasca in humans – An overview focusing on developmental toxicology. J Psychoactive Drugs. 2013;45(1):68–78.
37 Hoelen DWM, Spiering W, Valk GD. Long-QT syndrome induced by the antiaddiction drug ibogaine. N Engl J Med. 2009;360(3):308–9.
38 Paling FP, Andrews LM, Valk GD, Blom HJ. Life-threatening complications of ibogaine: three case reports. Neth J Med. 2012;70(9):422–4.
39 Alper KR, Stajić M, Gill JR. Fatalities temporally associated with the ingestion of ibogaine. J Forensic Sci. 2012;57(2):398–412.
40 Fantegrossi WE, Murnane KS, Reissig CJ. The behavioral pharmacology of hallucinogens. Biochem Pharmacol. 2008;75(1):17–33.
41 Nichols DE. Hallucinogens. Pharmacol Ther. 2004;101(2):131–81.
42 Parrott AC. Human psychobiology of MDMA or “Ecstasy”: an overview of 25 years of empirical research. Hum Psychopharmacol. 2013;28(4):289–307.
43 Parrott AC. The potential dangers of using MDMA for psychotherapy. J Psychoactive Drugs. 2014;46(1):37–43.
44 Loizaga-Velder A, Verres R. Therapeutic effects of ritual ayahuasca use in the treatment of substance dependence - Qualitative results. J Psychoactive Drugs. 2014;46(1):63–72.
45 Alper KR. Ibogaine: a review. Alkaloids Chem Biol. 2001;56:1–38.
46 Lotsof HS, Wachtel B, eds. Manual for ibogaine therapy screening, safety, monitoring and aftercare, Second Revision [Internet]. The Ibogaine Dossier; 2003. Available from: http://www.ibogaine.desk.nl/Ibogaine.pdf.
47 Schak KM, Vande Voort JL, Johnson EK, Kung S, Leung JG, Rasmussen KG, et al. Potential Risks of Poorly Monitored Ketamine Use in Depression Treatment. Am J Psychiatry. 2016;173(3):215–8.
48 Majić T, Schmidt TT, Gallinat J. Peak experiences and the afterglow phenomenon: when and how do therapeutic effects of hallucinogens depend on psychedelic experiences? J Psychopharmacol (Oxford). 2015;29(3):241–53.
49 Gasser P. Die psycholytische Psychotherapie in der Schweiz von 1988–1993: Eine katamnestische Erhebung. Swiss Archives of Neurology and Psychiatry. 1997;147(2):59–65.
50 Grob CS, Danforth AL, Chopra GS, Hagerty M, McKay CR, Halberstadt AL, et al. Pilot study of psilocybin treatment for anxiety in patients with advanced-stage cancer. Arch Gen Psychiatry. 2011;68(1):71–8.
51 Mithoefer MC, Grob CS, Brewerton TD. Novel psychopharmacological therapies for psychiatric disorders: psilocybin and MDMA. Lancet Psychiatry. 2016;3(5):481–8.
52 Carhart-Harris RL, Bolstridge M, Rucker J, Day CMJ, Erritzoe D, Kaelen M, et al. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. 2016;3(7):619–27.
53 Johnson MW, Garcia-Romeu A, Cosimano MP, Griffiths RR. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J Psychopharmacol (Oxford). 2014;28(11):983–92.
54 Garcia-Romeu A, Griffiths RR, Johnson MW. Psilocybin-occasioned mystical experiences in the treatment of tobacco addiction. Curr Drug Abuse Rev. 2014;7(3):157–64.
55 Bogenschutz MP, Forcehimes AA, Pommy JA, Wilcox CE, Barbosa PCR, Strassman RJ. Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study. J Psychopharmacol (Oxford). 2015;29(3):289–99.
56 Leonard HL, Rapoport JL. Relief of obsessive-compulsive symptoms by LSD and psilocin. Am J Psychiatry. 1987;144(9):1239–40.
57 Moreno FA, Wiegand CB, Taitano EK, Delgado PL. Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J Clin Psychiatry. 2006;67(11):1735–40.
58 Kast EC, Collins VJ. Study of lysergic acid diethylamide as an analgesic agent. Anesth Analg. 1964;43:285–91.
59 Sewell RA, Halpern JH, Pope HG. Response of cluster headache to psilocybin and LSD. Neurology. 2006;66(12):1920–2.
60 Karst M, Halpern JH, Bernateck M, Passie T. The non-hallucinogen 2-bromo-lysergic acid diethylamide as preventative treatment for cluster headache: an open, non-randomized case series. Cephalalgia. 2010;30(9):1140–4.
61 Gasser P, Holstein D, Michel Y, Doblin R, Yazar-Klosinski B, Passie T, et al. Safety and efficacy of lysergic acid diethylamide-assisted psychotherapy for anxiety associated with life-threatening diseases. J Nerv Ment Dis. 2014;202(7):513–20.
62 Gasser P, Kirchner K, Passie T. LSD-assisted psychotherapy for anxiety associated with a life-threatening disease: a qualitative study of acute and sustained subjective effects. J Psychopharmacol (Oxford). 2015;29(1):57–68.
63 Krebs TS, Johansen PØ. Lysergic acid diethylamide (LSD) for alcoholism: meta-analysis of randomized controlled trials. J Psychopharmacol (Oxford). 2012;26(7):994–1002.
64 Shin LM, Rauch SL, Pitman RK. Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Ann N Y Acad Sci. 2006;1071:67–79.
65 Bouso JC, Doblin R, Farré M, Alcázar MA, Gómez-Jarabo G. MDMA-assisted psychotherapy using low doses in a small sample of women with chronic posttraumatic stress disorder. J Psychoactive Drugs. 2008;40(3):225–36.
66 Mithoefer MC, Wagner MT, Mithoefer AT, Jerome L, Doblin R. The safety and efficacy of {+/-}3,4-methylenedioxymethamphetamine assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study. J Psychopharmacol (Oxford). 2011;25(4):439–52.
67 Mithoefer MC, Wagner MT, Mithoefer AT, Jerome L, Martin SF, Yazar-Klosinski B, et al. Durability of improvement in post-traumatic stress disorder symptoms and absence of harmful effects or drug dependency after 3,4-methylenedioxymethamphetamine-assisted psychotherapy: a prospective long-term follow-up study. J Psychopharmacol (Oxford). 2013;27(1):28–39.
68 Oehen P, Traber R, Widmer V, Schnyder U. A randomized, controlled pilot study of MDMA (± 3,4-Methylenedioxymethamphetamine)-assisted psychotherapy for treatment of resistant, chronic Post-Traumatic Stress Disorder (PTSD). J Psychopharmacol (Oxford). 2013;27(1):40–52.
69 Danforth AL, Struble CM, Yazar-Klosinski B, Grob CS. MDMA-assisted therapy: A new treatment model for social anxiety in autistic adults. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:237–49.
70 Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, et al. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry. 2000;47(4):351–4.
71 Zarate CA, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63(8):856–64.
72 Diazgranados N, Ibrahim L, Brutsche NE, Newberg A, Kronstein P, Khalife S, et al. A randomized add-on trial of an N-methyl-D-aspartate antagonist in treatment-resistant bipolar depression. Arch Gen Psychiatry. 2010;67(8):793–802.
73 Price RB, Nock MK, Charney DS, Mathew SJ. Effects of intravenous ketamine on explicit and implicit measures of suicidality in treatment-resistant depression. Biol Psychiatry. 2009;66(5):522–6.
74 Diamond PR, Farmery AD, Atkinson S, Haldar J, Williams N, Cowen PJ, et al. Ketamine infusions for treatment resistant depression: a series of 28 patients treated weekly or twice weekly in an ECT clinic. J Psychopharmacol (Oxford). 2014;28(6):536–44.
75 Singh JB, Fedgchin M, Daly EJ, De Boer P, Cooper K, Lim P, et al. A double-blind, randomized, placebo-controlled, dose-frequency study of intravenous ketamine in patients with treatment-resistant depression. Am J Psychiatry. 2016;173(8):816–26.
76 Lapidus KAB, Levitch CF, Perez AM, Brallier JW, Parides MK, Soleimani L, et al. A randomized controlled trial of intranasal ketamine in major depressive disorder. Biol Psychiatry. 2014;76(12):970–6.
77 Schoevers RA, Chaves TV, Balukova SM, Rot MAH, Kortekaas R. Oral ketamine for the treatment of pain and treatment-resistant depression. Br J Psychiatry. 2016;208(2):108–13.
78 Kishimoto T, Chawla JM, Hagi K, Zarate CA, Kane JM, Bauer M, et al. Single-dose infusion ketamine and non-ketamine N-methyl-d-aspartate receptor antagonists for unipolar and bipolar depression: a meta-analysis of efficacy, safety and time trajectories. Psychol Med. 2016;46(7):1459–72.
79 Zhang MW, Harris KM, Ho RC. Is off-label repeat prescription of ketamine as a rapid antidepressant safe? Controversies, ethical concerns, and legal implications. BMC Med Ethics. 2016;17:4.
80 Feder A, Parides MK, Murrough JW, Perez AM, Morgan JE, Saxena S, et al. Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2014;71(6):681–8.
81 Krupitsky EM, Grinenko AY. Ketamine psychedelic therapy (KPT): a review of the results of ten years of research. J Psychoactive Drugs. 1997;29(2):165–83.
82 Krupitsky E, Burakov A, Romanova T, Dunaevsky I, Strassman R, Grinenko A. Ketamine psychotherapy for heroin addiction: immediate effects and two-year follow-up. J Subst Abuse Treat. 2002;23(4):273–83.
83 Sessa B, Johnson MW. Can psychedelic compounds play a part in drug dependence therapy? Br J Psychiatry. 2015;206(1):1–3.
84 Thomas G, Lucas P, Capler NR, Tupper KW, Martin G. Ayahuasca-assisted therapy for addiction: results from a preliminary observational study in Canada. Curr Drug Abuse Rev. 2013 Mar;6(1):30–42.
85 Brierley DI, Davidson C. Developments in harmine pharmacology--implications for ayahuasca use and drug-dependence treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2012 Dec 3;39(2):263–72.
86 Liester MB, Prickett JI. Hypotheses regarding the mechanisms of ayahuasca in the treatment of addictions. J Psychoactive Drugs. 2012 Aug;44(3):200–8.
87 Osório FL, Sanches RF, Macedo LR, Santos RG dos, Maia-de-Oliveira JP, Wichert-Ana L, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a preliminary report. Rev Bras Psiquiatr. 2015 Mar;37(1):13–20.
88 He D-Y, McGough NNH, Ravindranathan A, Jeanblanc J, Logrip ML, Phamluong K, et al. Glial cell line-derived neurotrophic factor mediates the desirable actions of the anti-addiction drug ibogaine against alcohol consumption. J Neurosci. 2005 Jan 19;25(3):619–28.
89 Glick SD, Maisonneuve IM, Szumlinski KK. 18-Methoxycoronaridine (18-MC) and ibogaine: comparison of antiaddictive efficacy, toxicity, and mechanisms of action. Ann N Y Acad Sci. 2000 Sep;914:369–86.
90 Alper KR, Lotsof HS. The use of ibogaine in the treatment of addictions. In: Winkelman M, Roberts TB, editors. Psychedelic Medicine: : New Evidence for Hallucinogenic Substances as Treatments 2 Vols. 1st ed. Westport, CT: Praeger Publishers; 2007. p. 43-66.
91 Brown TK. Ibogaine in the treatment of substance dependence. Curr Drug Abuse Rev. 2013 Mar;6(1):3–16.
92 Alper KR, Lotsof HS, Frenken GM, Luciano DJ, Bastiaans J. Treatment of acute opioid withdrawal with ibogaine. Am J Addict. 1999;8(3):234–42
93 Mash D, Kovera CA, Pablo J, Tyndale RF, Ervin FD, Williams IC, et al. Ibogaine: Complex Pharmacokinetics, Concerns for Safety, and Preliminary Efficacy Measures. Ann N Y Acad Sci. 2000 Sep;914:394-401.
94 Mash DC, Kovera CA, Pablo J, Tyndale R, Ervin FR, Kamlet JD, et al. Ibogaine in the treatment of heroin withdrawal. Alkaloids Chem Biol. 2001;56:155–71.
95 Glick SD, Maisonneuve IM. Development of novel medications for drug addiction. The legacy of an African shrub. Ann N Y Acad Sci. 2000;909:88–103.
96 Chang Q, Hanania T, Mash DC, Maillet EL. Noribogaine reduces nicotine self-administration in rats. J Psychopharmacol (Oxford). 2015 Jun;29(6):704–11.
97 1971 Convention on Psychotropic Substances, 9 December 1975, A/RES/3443, UN General Assembly, available at: http://www.refworld.org/docid/3b00f1ad4b.html
98 Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. 2007 Mar 24;369(9566):1047–53.
99 Nutt DJ, King LA, Phillips LD, Independent Scientific Committee on Drugs. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010 Nov 6;376(9752):1558–65.
100 Krebs TS, Johansen P-Ø. Psychedelics and mental health: a population study. PLoS ONE. 2013;8(8):e63972.
101 Johansen P-Ø, Krebs TS. Psychedelics not linked to mental health problems or suicidal behavior: A population study. J Psychopharmacol (Oxford). 2015 Mar 5; 29(3):270-279.
102 Hendricks PS, Thorne CB, Clark CB, Coombs DW, Johnson MW. Classic psychedelic use is associated with reduced psychological distress and suicidality in the United States adult population. J Psychopharmacol (Oxford). 2015 Mar;29(3):280–8.